| Issue Brief |
Medicare’s Financial Condition: Beyond Actuarial Balance |
|
APRIL 2019 |
|
Download a PDF version here. Each year, the Boards of Trustees of the Federal Hospital Insurance (HI) and Supplementary Medical Insurance (SMI) trust funds submit a report to Congress on the Medicare program’s financial condition. The program is operated through two trust funds. The HI trust fund (Medicare Part A) pays primarily for inpatient hospital services. The SMI trust fund includes accounts for the Medicare Part B program, which covers physician and outpatient hospital services, and the Medicare Part D program, which covers the prescription drug program. The Medicare Trustees Report is the primary source of information on the financial status of the Medicare program, and the American Academy of Actuaries proudly recognizes the important contribution that members of the actuarial profession have made in preparing the report. The Academy members play a vital role in providing information to the public about the important issues surrounding the program’s solvency and sustainability. The 2019 Medicare Trustees Report finds that compared with the projections from the 2018 report, the projected financial condition of Medicare has deteriorated in the short term for parts A and B and improved for part D.1 The HI trust fund is now projected to be depleted in 2026, the same as in last year’s report. This leaves policymakers only seven years to find a solution. |
The program faces three fundamental long-range financing challenges:
- Income to the HI trust fund is not adequate to fund the HI portion of Medicare benefits;
- Increases in SMI costs increase pressure on beneficiary household budgets and the federal budget; and
- Increases in total Medicare spending threaten the program’s sustainability.
The trustees conclude: “The projections in this year’s report continue to demonstrate the need for timely and effective action to address Medicare’s remaining financial challenges—including the projected depletion of the HI trust fund, this fund’s long-range financial imbalance, and the rapid growth in Medicare expenditures."
In this issue brief, the American Academy of Actuaries’ Medicare Subcommittee examines the findings of the Medicare Trustees Report with respect to program solvency and sustainability. The Medicare program continues to face serious financing problems. Due to Medicare’s critically important role in ensuring that Americans age 65 and older and certain younger adults with permanent disabilities have access to health care, it is important for policymakers to address the challenges that threaten the program’s long-term solvency and financial sustainability. The longer corrective measures are delayed, the worse the financial challenges will become and in turn, the greater the burden that is likely imposed on beneficiaries and taxpayers.
Medicare HI Trust Fund Income Falls Short of the Amount Needed To Fund HI Benefits
Medicare’s trust funds account for all income and expenditures. The HI and SMI programs operate separate trust funds with different financing mechanisms. General revenues, payroll taxes, premiums, and other income are credited to the trust funds, which are used to pay benefits and administrative costs. Any unused income is required by law to be invested in U.S. government securities for use in future years. In effect, the trust fund assets represent loans to the U.S. Treasury’s general fund.
The HI trust fund, which pays for hospital services, is funded primarily through earmarked payroll taxes.
The projections of Medicare’s financial outlook in the report are based on current law. The projected HI trust fund exhaustion date is 2026, unchanged from last year’s Medicare Trustees Report. However, the 75-year HI deficit increased—from 0.82 percent of taxable payroll in the 2018 report to 0.91 percent in this year’s report. The increase primarily reflects lower assumed productivity growth, higher costs and lower income in 2018 than expected, and lower real discount rates, offset somewhat by slower projected growth in the utilization of skilled nursing facility services.
- HI expenditures are projected to exceed HI revenues. After experiencing small surpluses in 2016 and 2017, a deficit returned in 2018. HI expenditures are expected to exceed revenues, including interest income, in every year during the 75-year projection period. As a result, the HI trust fund assets will need to be redeemed. When the federal government is experiencing unified budget deficits, funding the redemptions requires that additional money be borrowed from the public, thereby increasing the federal deficit and debt.
- The HI trust fund is projected to be depleted in 2026. At that time, tax revenues are projected to cover only 89 percent of program costs, with the share declining to 77 percent in 2046 and then increasing to 83 percent in 2093. There is no current provision allowing for general fund transfers to cover HI expenditures in excess of dedicated revenues.
- The projected HI deficit over the next 75 years is 0.91 percent of taxable payroll. Eliminating this deficit would require an immediate 31 percent increase in standard payroll taxes or an immediate 19 percent reduction in expenditures—or some combination of the two. Delaying action would require more severe changes in the future.
The trustees acknowledge that the estimates based on current law projections could understate the seriousness of Medicare’s financial condition, because actual Medicare expenses might exceed current law estimates. In particular, the trustees and the chief actuary point to scheduled reductions in provider payments that may not occur. Current law requires downward adjustments in payment updates for most non-physician providers to reflect productivity improvements; these adjustments might not be sustainable in the long term. Current law also requires updates for physician services that are not expected to keep up with physician costs. In the Statement of Actuarial Opinion that accompanies the report, the chief actuary of the Centers for Medicare & Medicaid Services (CMS) specifically states, “Should these price updates prove to be inadequate, beneficiaries’ access to and the quality of Medicare benefits would deteriorate over time, or future legislation would need to be enacted that would likely increase program costs beyond those projected under current law in this report.”
At the request of the trustees, the CMS Office of the Actuary developed an alternative analysis that provides an illustration of the potential understatement of current-law Medicare cost projections if the productivity adjustments were phased down gradually beginning in 2028 and physician updates were more consistent with cost growth. Although the illustrative alternative projections are not intended to be interpreted as the official best estimates of future Medicare costs, they do, as noted in the trustees’ report, “help illustrate and quantify the potential magnitude of the cost understatement.”
Under the alternative scenario, the HI trust fund still would be depleted in 2026. However, the projected deficit over the next 75 years would be 1.74 percent of taxable payroll—compared to 0.91 percent under current law. Eliminating this deficit would require an immediate 60 percent increase in standard payroll taxes or a 30 percent reduction in expenditures—or some combination of the two.
Increases in SMI Costs Increase Pressure on Beneficiary Household Budgets and the Federal Budget
 The SMI trust fund includes accounts for the Medicare Part B program, which covers physician and outpatient hospital services, and the Medicare Part D program, which covers the prescription drug program. Approximately one-quarter of SMI spending is financed through beneficiary premiums, with federal general tax revenues covering the remaining three-quarters.2
The SMI trust fund includes accounts for the Medicare Part B program, which covers physician and outpatient hospital services, and the Medicare Part D program, which covers the prescription drug program. Approximately one-quarter of SMI spending is financed through beneficiary premiums, with federal general tax revenues covering the remaining three-quarters.2
The SMI trust fund is expected to remain solvent due to its financing being reset each year to meet projected future costs. As a result, increases in SMI costs will require increases in beneficiary premiums and general revenue contributions. Increases in general revenue contributions will put more pressure on the federal budget. SMI general revenue funding is scheduled to nearly double from 1.6 percent of gross domestic product (GDP) in 2019 to 3.0 percent in 2093.
Premium increases similarly will increase the burden on beneficiaries, especially when considered in conjunction with increasing beneficiary cost-sharing expenses. The average beneficiary expenses (premiums and cost-sharing) for parts B and D combined are currently 23 percent of the average Social Security benefit. These expenses are projected to increase to 35 percent of the average Social Security benefit by 2093. These expenses do not include cost sharing under Part A.
The 2019 Medicare Trustees Report projects that total SMI spending will continue to grow faster than GDP. The total spending will increase from 2.1 percent of GDP in 2018 to 3.2 percent of GDP in 2030 and to 4.2 percent of GDP in 2093.
Spending under the illustrative alternative analysis would be higher, especially in the long term, reflecting the phase-down of productivity adjustments for non-physician provider payments and higher physician updates in the long range. SMI spending projected in the alternative analysis would increase from 2.1 percent of GDP in 2018 to 3.3 percent of GDP in 2030 and to 5.6 percent of GDP in 2093.
Increases in Total Medicare Spending Threaten the Program’s Sustainability
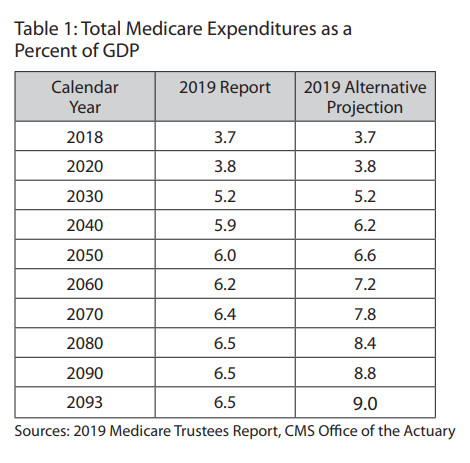
A broader issue related to Medicare’s financial condition is whether the economy can sustain Medicare spending in the long run. To help gauge the future sustainability of the Medicare program, the trustees consider the share of GDP that will be consumed by Medicare. With Medicare spending expected to continue growing faster than GDP, greater shares of the economic growth will be devoted to Medicare over time, meaning smaller shares of the economy will be available for other priorities.Under current law, Medicare expenditures as a percentage of GDP will grow from 3.7 percent of GDP in 2018 to 6.5 percent of GDP in 2093. However, under the CMS Office of the Actuary alternative scenario, total Medicare expenditures would increase to 9.0 percent of GDP in 2093.
Conclusion
Consistent with prior reports, the 2019 Medicare Trustees Report stresses the serious financial challenges facing the Medicare program. The HI trust fund is projected to be depleted in 2026—the same as projected in last year’s report—and the 75-year HI deficit has grown. Medicare spending will continue to grow faster than the economy—increasing the pressure on beneficiary household budgets, the federal budget, and threatening the program’s sustainability.
As noted by the trustees, Medicare’s financial challenges could be more severe than projected under current law assumptions. The report’s Medicare spending projections are considered understated to the extent that the ACA’s provisions for downward adjustments in non-physician provider payment updates to reflect productivity improvements and long-range physician payment updates being held below physician costs are unsustainable in the long term. If Medicare projections are calculated using assumptions that the productivity adjustments are phased down and physician updates are more in line with their costs, Medicare’s financial condition is shown to be even worse than under the projected baseline.
The trustees note the urgency of addressing Medicare’s financial challenges, stating:
The Board of Trustees believes that solutions can and must be found to ensure the financial integrity of HI in the short and long term and to reduce the rate of growth in Medicare costs through viable means. The sooner the solutions are enacted, the more flexible and gradual they can be. Moreover, the early introduction of reforms increases the time available for affected individuals and organizations—including health care providers, beneficiaries, and taxpayers—to adjust their expectations and behavior. The Board recommends that Congress and the executive branch work together with a sense of urgency to address these challenges.
Medicare’s challenges are not solely financial. Medicare beneficiaries are a diverse group with diverse health care needs and certain beneficiary populations, such as those with a disability or multiple chronic conditions, are particularly vulnerable to having high health care needs. Many beneficiaries have limited resources to rely upon should they be faced with high out-of-pocket health costs. Aside from the addition of the prescription drug program in 2006, Medicare’s fee-for-service benefit package has remained mostly unchanged; some services aren’t covered and beneficiary out-of pocket costs are not capped. Therefore, any changes aiming to improve Medicare’s financial condition should be considered in light of how the changes would impact the program’s ability to meet the health care needs of beneficiaries and whether the changes would encourage beneficiaries to seek cost-effective care.
|
Craig Hanna, Director of Public Policy Members of the Medicare Subcommittee include: Michael Thompson, MAAA, FSA—Chairperson; John Bertko, MAAA, FSA; Jill H. Brostowitz, MAAA, FSA; Puneet Budhiraja, MAAA, ASA; Jennifer Carioto, MAAA, FSA; Michael V. Carstens, MAAA, FSA; April S. Choi, MAAA, FSA; Gabriela Dieguez, MAAA, FSA; Randall S. Edwards, MAAA, FSA; Troy M. Filipek, MAAA, FSA, FCA; Brandon Flowers, MAAA, FSA; Robert Garbus, MAAA, ASA; Dustin Grzeskowiak, MAAA, ASA; Katherine Holcomb, MAAA, FSA; Siliang Hu, MAAA, ASA; Dennis J. Hulet, MAAA, FSA, FCA; Craig Huval, MAAA, ASA; Joel C. Kabala, MAAA, ASA; Margot D. Kaplan, MAAA, FCA, ASA; Michael Krentzman, MAAA, ASA; Katherine LaCalamita, MAAA, FSA; Julia Lambert, MAAA, FSA; Li Lee, MAAA, FSA; Jinn-Feng Lin, MAAA, FSA, FCA; Joe Liss, MAAA, FSA; Mark E. Litow, MAAA, FSA; Marilyn McGaffin, MAAA, ASA; Bob Mone, MAAA, FSA; Mary Murley, MAAA, ASA; Catherine Murphy-Barron, MAAA, FSA; Steve Niu, MAAA, FSA, EA; Donna Novak , MAAA, FCA, ASA; Vanessa Olson, MAAA, FSA; Susan E. Pierce, MAAA, FSA; Robert J. Pipich, MAAA, FSA; Anna M. Rappaport, MAAA, FSA, EA; Jeremiah D. Reuter, MAAA, ASA; Geoff Sandler, MAAA, FSA; John Schubert, MAAA, FCA, ASA; Andrea Sheldon, MAAA, FSA; Derek Skoog, MAAA, FSA; Joshua Sober, MAAA, FSA; Maureen Tresnak, MAAA, FSA; Cori E. Uccello, MAAA, FSA, FCA, MPP; John A. Wandishin, MAAA, FSA; Thomas F. Wildsmith, MAAA, FSA. © 2019 American Academy of Actuaries. All rights reserved. |







